Abstract
This article reports the findings of a study into the information given to women about hormone replacement therapy (HRT) and the prevention of osteoporosis. The author examines the reasons for prescription of HRT and why some women discontinue the treatment before a preventative effect is likely to have taken place. The study found a lack of appropriate information being given by health professionals to enable women to consider their overall postmenopausal health and recommends a review of the content of information given on the subject.
From the author's experience as a sister on an orthopaedic ward, it seemed that many patients prescribed hormone replacement therapy (HRT) were not aware of the reasons for continuing the therapy in the longer term, and therefore, often stopped taking the treatment prematurely, before osteoporosis was likely to be prevented.
Literature Review
A review of the literature demonstrated that it is generally accepted that the main determinant of peak bone density is genetic. Smith et al (1973) found that bone density varied much less between identical than non-identical twins. Researchers are also in agreement that following cessation of ovarian function at the menopause, bone is lost at an accelerated rate. Stephenson (1989) showed that peak bone density is achieved at the end of skeletal growth, at approximately age 30 in women. However, following cessation of ovarian function at the menopause, bone is lost from the spine at the rate of 5 per cent per year for five to ten years (Abdallah et al 1984). The rate of loss is even higher for women who have had bilateral oophorectomy.
Researchers vary in their opnions as to how oestrogen may affect bone. Hillyard et al (1978) suggested that oestrogen may have an indirect effect via calcitonin. Garn (1975) supported this theory by suggesting that racial differences in calcitonin levels would explain why black women have lower incidences of osteoporosis.
Many studies have shown an increase in the rate of osteoporotic fractures in the past 30 years. Obrant et al (1989) concluded that this was likely to be due to a decline in physical activity, particularly work-related activity, and the population's increased dependance on motorised transport. In addition to sedentary lifestyle and loss of ovarian function, several other factors have been identified as being risk factors for osteoporosis. These include (Jenson et al 1982):
- Family history,
- Cigarette smoking,
- Increased alcohol intake,
- Inadequate childhood nutrition,
- Being underweight.
Osteoporosis often used to be dismissed as a normal part of ageing, however, researchers are now in agreement that with the advent of accurate and precise measurement of bone density and the identification of risk factors, the ability to manage osteoporosis has been transformed (Melton et al 1990).
Researchers also agree that the two main factors which determine whether or not a woman will develop osteoporosis are her maximum premenopausal skeletal mass and the amount of bone she subsequently loses (Smith et al 1973). Some suggestions have been made as to how peak bone density can be improved; these include encouraging a high intake of dairy products in childhood and adolescence (Sandler et al 1985), abd promoting the benefits of physical activity in the population as a whole (Cooper et al 1988).
Many doctors now agree that HRT is an effective method of preventing osteoporosis and many believe that it should be available to all women at the time of the menopause (National Osteoporosis Society 1992). The National Osteoporosis Society suggest that HRT should last for ten years in order to prevent osteoporosis.
As research has shown that most women undergo HRT for control of the symptoms of the menopause (Hunt 1988), they may be unaware of the benefits of continuing HRT once their symptoms have subsided. Cook (1991) showed that women who were given information about the risks of osteoporosis were more likely to make positive lifestyle changes.
There appear to be no references to research which asked whether women undergoing HRT were aware of the benefits of continuing long-term therapy in order to prevent osteoporosis. Based on this apparent lack of information, the author proposed the research question:
'What do women in one general practice who have been prescribed HRT know about osteoporosis?
This was subdivided into four subquestions:
- Were the women aware that osteoporosis is a serious condition?
- Were the women aware that HRT can prevent osteoporosis, and if so, where did they obtain this information?
- Were the women aware of the length of time that HRT needs to be taken to prevent osteoporosis?
- Were there any side-effects of HRT that may cause the women to discontinue the therapy?
Methodology
A quantative style of research was adopted. In order to ensure patient confidentiality, a questionnaire was used to collect data. The research proposal was approved by the local ethics committee.
The sample selected for this research was all women prescribed HRT in one general practice in Scarborough, and as such, the results may not be representative of the population as a whole and cannot be legitmately generalised.
Results and Discussion
A total of 77 questionnaires were sent to patients and 43 were returned, a response rate of 57 per cent. The mean age when women were first prescribed HRT was 49 years, the youngest being 30 years old and the oldest 62 years old. Only three respondents were outside the age range of 40 to 55 years when first prescribed the therapy. Most were, therefore, at an age where they were possibly encountering problems with the menopause.
Twenty three per cent of the respondents had been given no reason for undergoing HRT. The remainder had been prescibed HRT for menopausal symptoms. Only 24 per cent of the sample were told that HRT could prevent osteoporosis.
Most of the women were not advised specifically to continue the therapy for five to ten years and they are, therefore, at risk of developing osteoporosis if they do not obtain this information elsewhere (Abdallah et al 1984).
These findings indicate that the practice needs to review the information given to women concerning the length of time they should continue HRT.
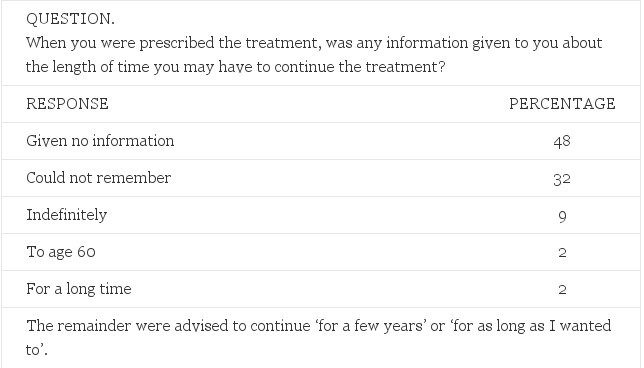
Table 1. Advice given to women on how long to continue HRT
An interesting finding on analysing the questionnaires was that 95 per cent of the respondents were aware that HRT could prevent osteoporosis. Of these, 88 per cent had received this information from the mass media with only 24 per cent receiving the information from a healthcare professional. Some women had received information from more than one source.
The respondents believed the prevention of osteopororsis to be important. The importance that the women placed on preventing osteoporosis was significantly higher than nay other reason for taking HRT. the mean score on the Likert Scale for the importance of taking HRT was 4.6 (the maximum score being 5). Hot flushes scored 4, preventing vaginal dryness scored 3.1.
The fourth subquestion of the research was to discover if there were any side-effects of HRT which may cause women to discontinue the therapy. This information was gained in two ways: first, the women were asked if they had been made aware of any possible side-effects by their prescribing doctor, as this information may have enabled the women to recognise any side-effects when they developed; second, the women were asked if they had expereinced any side-effects and whether they had considered stopping the therapy as a result. The responses showed that:
- 60% were given no information about possible side-effects.
- 16% were told that they may experience side-effects including menstrual bleeding, weight gain, voice change, reduction in breast size and headaches.
(The remainder (34 per cent) could not remember or did not answer the question).
- 53% had suffered no side-effects.
- 26% of respondents had considered stopping the therapy as their symptoms had subsided.
- 17% of respondents considered stopping because the symptoms for which they were originally prescribed the treatment were not subsiding.
There was no statistical difference in experience of side-effects between the women who had been warned of possible side-effects and those who had not. Of the women who had been given appropriate advice on how long to continue HRT, fewer had considered stopping. This finding is supported by the fact that 8 per cent had considered stopping the therapy because they were unaware of the need to continue it.
An unexpected finding was that a further 8 per cent said that the cost of prescriptions was prohibitive to their continuing the therapy.
Conclusion
This research identifies that most women who are prescibed HRT in the group practice and who responded to the questionnaire are prescibed HRT for the control of the symptoms of menopause. The women are mostly aware that HRT can prevent osteoporosis and they consider the prevention of osteoporosis an important reason for taking the therapy.
- The reasons for prescribing the drug.
- Possible alternatives including dietary and lifestyle measures.
- Side-effects of the treatment.
- How long the treatment should continue.
Box 1. List of information women should be given when prescribed HRT
Most of the women had not been given information about osteoporosis from a health professional, but had gleaned the information from the mass media. Most of the women had not been advised how long to continue the therapy. Those who were not advised were most likely to stop the therapy before osteoporosis was likely to have been prevented.
The findings identify the need for the practice to consider the information it gives to patients prescribed HRT, to enable them to make informed decisions about continuing the therapy (Box 1).
Implications for practice
- Patients require detailed information about HRT to enable them to make informed decisions about continuation of treatment in the face of increasing side-effects.
- Nurses should be aware of all the benefits and side-effects of HRT to enable them to fulfill their role as patient educators.
- Further research is required to verify the results of this study and to establish how many women are aware of the preventive benefits of HRT in relation to osteoporosis.
- Due to advances in treatment, osteoporosis should no longer be seen as a normal part of ageing.
© Dianne Swiers (RGN, ONC, BSc(Hons), DPSN, PGCE) 1996; Nursing Standard; 10; 26; 35-37.
References
- Abdallah H et al (1984) cited in Christiansen C et al (1984) Osteoporosis 1984. Copenhagen, Glostrup Hospital.
- Cook B et al (1991) An osteoporosis patient education and screening programme. Patient Education and Counselling. 17; 2; 135-145.
- Cooper C et al (1988) Physical activity, muscle strength and calcium intake. British Medical Journal. 297; 1443-1446.
- Garn SM (1975)Bone Loss and Aging. New York NY, Academic Press.
- Hillyard CJ et al (1978) Relative deficiency of plasma calcitonin in normal women. Lancet. 1; 8071; 961-962.
- Hunt K (1988) Perceived value of treatment among a group of long term users of hormone replacement therapy. Journal College of General Practioners. 38; 398-401.
- Jensen GF et al (1982) Epidemiology of post menopausal spinal and long bone fractures. Clinical Orthopaedic and Related Research. 166; 75-81.
- Melton LJ et al (1990) Screening for osteoporosis. International Medical Journal. 112; 516-528.
- National Osteoporosis Society (1992) National Osteoporosis and Hormone Replacement Therapy. Bath, National Osteoporosis Society.
- Obrant KJ et al (1989) Increased age adjusted risk of fragility fractures. Calcified Tissue Journal. 44; 157-162.
- Sandler RB et al (1985) Post menopausal bone density and milk consumption in childhood and adolescence. American Journal of Clinical Nutrition. 41; 270-274.
- Smith DM et al (1973) Genetic factors in determining bone mass. Journal of Clinical Medicine. 52; 2800-2808.
- Stephenson JC (1989) New Techniques in Metastatic Bone Disease. London, Wright.
Comments
comments powered by Disqus